Medical Decision Making TIP #3
MDM Tip #3
An overview of the revised MDM
Medical Decision Making: selecting the correct level of service for codes 99202—99215 in 2021:
- In 2021, E/M codes 99202—99215 will have a changed definition of MDM
- The new MDM Chart is similar to the current table of risk, but with significant changes, particularly in data
- Finally! Definitions of key terms in MDM
CPT® is simplifying code selection for new and established patient office or other outpatient E/M services in 2021. CPT® heard the complaints of physicians and other clinicians about counting bullets, about reviewing systems that aren’t relevant to the presenting problem, or being asked to document the family history on a 90-year-old patient, when billing a high-level service for a complex or seriously ill patient. Beginning in 2021, for codes 99202–99215, history and exam are no longer required components in code selection. CPT® says “the nature and extent of the history and or physical examination is determined by the treating physician or other qualified health care professional.”
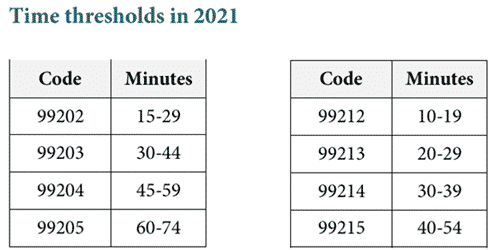
In 2021, these codes may be selected by either the level of medical decision-making as defined for each service, or by the total time for E/M services performed on the date of encounter.
Medical decision-making is paramount
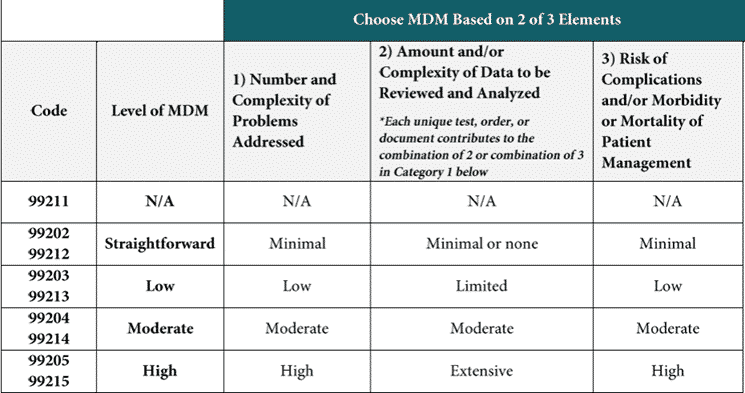
Many clinicians have wanted to use the severity of the patient’s illness and the risks related to the illness and treatment to select the level of service. They are now getting their wish. Medical decision-making will be determined by the following three elements:
- the number and complexity of problem(s) that are addressed during the encounter,
- the amount and/or complexity of data to be reviewed and analyzed, and
- the risk of complications, morbidity, and/or mortality of patient management decisions made at the visit, associated with the patient’s problem(s), or treatment(s).
This sounds familiar to us, and familiar to anyone who has used the point system. The point system came from an audit sheet developed by the Marshfield Clinic (not included in the original guidelines) and implemented by many payers. However, although the framework for determining medical decision-making will seem familiar, there are key differences, particularly in the area of data. In addition, the revised 2021 CPT® book has added very helpful definitions to the section on E/M services to the 2021 CPT® book. These definitions provide clarity for coders and clinicians alike in the interpretation of medical decision-making.
CPT® has released a single page chart that can be used in assessing the level of medical decision-making.
The MDM for a 99212 is exactly equivalent to the MDM required for a 99202. Similarly, 99213 and 99203 have the same requirements,99214 and 99204 have the same requirements, and 99215 and 99205 have the same requirements.
There are four levels of medical decision-making: straightforward, low, moderate, and high. In order to attain that level of MDM, two out of the three elements (the number of complexity and problems addressed, the amount and/or the complexity of data reviewed and analyzed, and the risk of complications and/or morbidity or mortality of patient management).
When billing for interpreting a test
CPT® is clarifying that if the physician, physician assistant, or nurse practitioner is reporting, (that is billing for), the interpretation and/or report for a diagnostic test, it may not be counted as part of the data in determining the level of MDM. This question has plagued coders and auditors for as long as they have been coding E/M services. It’s helpful to have a definitive answer. An example might illustrate this more clearly than these words.
Example #1
A patient is seen in an urgent care center with cough, wheezing and fever. The physician orders a chest x-ray and provides a professional interpretation for the chest x-ray. The physician writes a separate report interpreting the results, and bills for globally for the interpretation of the x-ray. This could be with the modifier if only the professional component is performed, or could be billed globally and include both technical and professional component.
The distinction here is that if the professional component is being billed by the physician, the physician may not include reviewing the image as part of the determination of the amount of data to be reviewed. The physician is being paid for the interpretation, and so may not count reviewing the image as data complexity.
Example #2
That same patient is seen in follow-up by their primary care physician three days later. The primary care physician pulls up the image and looks at the chest x-ray. However, the primary care physician is not billing (reporting) the interpretation of the x-ray. The primary care physician may include independent visualization of the chest x-ray in determining the amount of data for medical decision-making.
Two of three MDM elements required
In order to select a level of service based on medical decision-making, two of the elements must be met. (The number and complexity of problems, amount and or complexity of data to be reviewed and analyzed, risk of complications and/or mortality of patient management.)