Medical Decision Making TIP #6
MDM Tip #6
The third element of MDM in 2021
The 3rd (of 3) elements of MDM: Risk of complications and/or morbidity or mortality of patient management
(Questions can be emailed to our ACS partners at: lsucoding@acsmd.com)
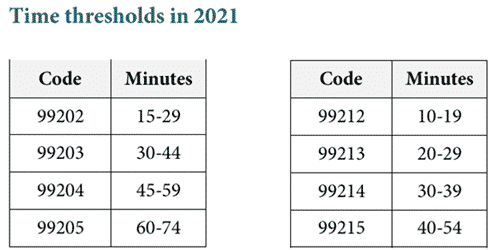
E/M changes for 2021 for codes 99202—99215
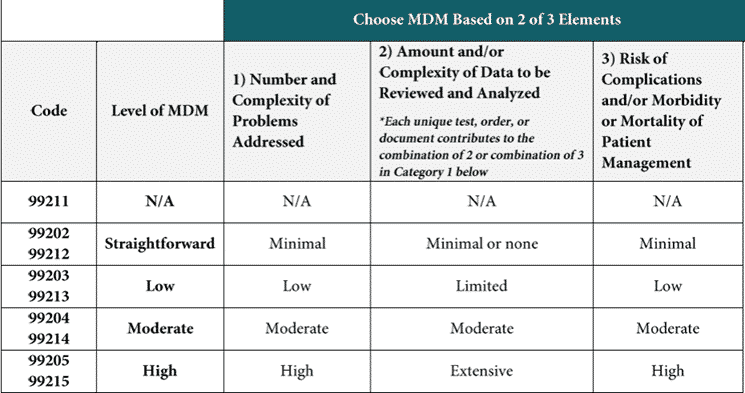
- There are three elements in medical decision-making and this article describes the third, the risk of complications and/or morbidity or mortality related to patient management
- When selecting a level of service based on medical decision-making two of the three elements are required
- CPT® has developed definitions for many of the components in the MDM chart and this article describes the definitions and rules related to morbidity and mortality.
Definitions related to data in the new MDM chart for office E/M visits in 2021
This article will start with the definitions and then describe how to select the level of morbidity/mortality related to patient treatment.
The CPT® definitions are in italics, my comments are not. (MDM chart)
Clinician’s determine risk, and do not need to explain their definitions of risk.
Risk: The probability and/or consequences of an event. The assessment of the level of risk is affected by the nature of the event under consideration. For example, a low probability of death may be high risk, whereas a high chance of a minor, self-limited adverse effect of treatment may be low risk. Definitions of risk are based upon the usual behavior and thought processes of a physician or other qualified health care professional in the same specialty. Trained clinicians apply common language usage meanings to terms such as ‘high’, ‘medium’, ‘low’, or ‘minimal’ risk and do not require quantification for these definitions, (though quantification may be provided when evidence-based medicine has established probabilities). For the purposes of medical decision making, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated. Risk also includes medical decision making related to the need to initiate or forego further testing, treatment and/or hospitalization.
- The clinician does not need to define or explain “minimal” risk, “low” risk, “moderate” risk and “high risk.” CPT® specifically states that these are common terms with a shared understanding of their meaning.
- These risk terms “do not require quantification for these definitions.”
- Risk is based upon the consequences of the problem.
- It also includes the decision making regarding initiating or foregoing further care.
Morbidity: A state of illness or functional impairment that is expected to be of substantial duration during which function is limited, quality of life is impaired, or there is organ damage that may not be transient despite treatment.
- Morbidity means having a disease or a symptom of a disease. It also refers to medical problems caused by the treatment.
- This element includes both, the morbidity of the disease itself and the morbidity/mortality of the treatment for the disease.
Social determinants of health: Economic and social conditions that influence the health of people and communities. Examples may include food or housing insecurity.
- Social determinants of health (SDoH) appears in moderate complexity, needed for codes 99204 and 99214. Moderate complexity may be defined as “diagnosis or treatment significantly limited by social determinants of health.” That’s new. A clinician may indicate that the patient is living in a shelter and doesn’t have access to a kitchen to follow a heart healthy diet needed for their condition. Or, a patient who is homeless could have a minor skin tear, the type of problem that would not normally qualify as moderate complexity, but without the ability for frequent dressing changes.
Drug therapy requiring intensive monitoring for toxicity: A drug that requires intensive monitoring is a therapeutic agent that has the potential to cause serious morbidity or death. The monitoring is performed for assessment of these adverse effects and not primarily for assessment of therapeutic efficacy. The monitoring should be that which is generally accepted practice for the agent, but may be patient specific in some cases.
Intensive monitoring may be long-term or short term. Long-term intensive monitoring is not less than quarterly. The monitoring may be by a lab test, a physiologic test or imaging. Monitoring by history or examination does not qualify. The monitoring affects the level of medical decision making in an encounter in which it is considered in the management of the patient.
Examples may include monitoring for a cytopenia in the use of an antineoplastic agent between dose cycles or the short-term intensive monitoring of electrolytes and renal function in a patient who is undergoing diuresis. Examples of monitoring that does not qualify include monitoring glucose levels during insulin therapy as the primary reason is the therapeutic effect (even if hypoglycemia is a concern); or annual electrolytes and renal function for a patient on a diuretic as the frequency does not meet the threshold.
- Finally, a definition for drug therapy requiring intensive monitoring!
- The monitoring is performed for assessment of adverse effects and not primary for assessment of therapeutic efficacy. If the purpose of the monitoring is to adjust the dosage of the medication, that is not considered intensive monitoring.
- The monitoring should be typical for that medication, although may be patient specific. An individual patient may have co-morbidities or be taking another medication that affects the need for intensive monitoring.
- The type of monitoring may be a lab test, physiologic test or imaging.
- Taking a history and doing an exam do not qualify as intensive monitoring.