Medical Decision Making TIP #4
MDM Tip #4
The first element of MDM in 2021 office visits
The 1st (of 3) elements of MDM: number and complexity of problems addressed
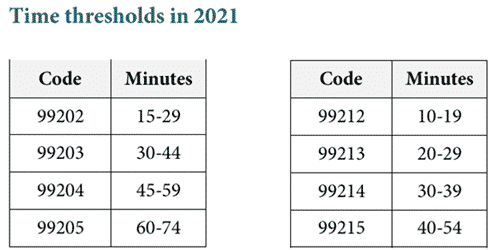
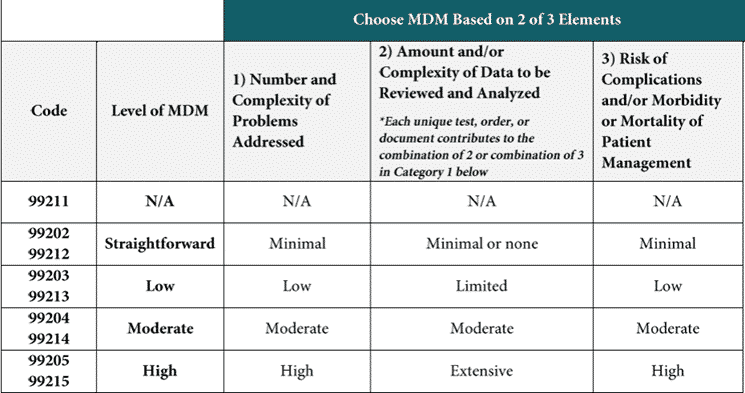
E/M changes for 2021 for codes 99202—99215
- There are three elements in medical decision-making and this article describes the first of three
- When selecting a level of service based on medical decision-making two of the three elements are required
- CPT® has developed definitions for many of the components in the MDM chart
This section of the revised guidelines, which will be printed in the CPT® book in 2021, starts by discussing problems and conditions that may be addressed in a single encounter.
- Multiple new or established conditions may be addressed at a single encounter, and will affect MDM.
- Symptoms of a condition that are related to specific diagnosis are not necessarily unique conditions. For example, a patient presents with fever, body aches, and cough, and the physician diagnosis influenza. The symptoms of the influenza are not considered unique conditions.
- CPT® clarifies that we should not consider comorbidities or underlying diseases unless they are address at the visit and their presence increases the amount and/or complexity of data that needs to be analyzed, or the risk of complications and or morbidity or mentality of patient management. Simply because a problem is mentioned on the problem list does not mean that we would assign it as a diagnosis code for an office or outpatient encounter. When assigning a diagnosis for an officer outpatient encounter, we follow the ICD-10 rule to code all documented conditions that require or affect patient care and management. Now, CPT® is clarifying that we should use a similar standard when determining the number of problems in the first element of MDM. If the clinician is either treating the condition or, the condition requires that the clinician review or order additional tests or notes, or if the comorbidity increases the risk of the treatment for the current problem, then we will credit it in this first element of MDM
- The final diagnosis for a condition does not equate with risk. An extensive evaluation many be required to evaluate a condition, even if the clinician reaches the conclusion that the signs or symptoms do not “represent a highly morbid condition.”
Definitions for E/M in 2021 related to problems
Problem: A problem is a disease, condition, illness, injury, symptom, sign, finding, complaint, or other matter addressed at the encounter, with or without a diagnosis being established at the time of the encounter.
- Keep in mind that symptoms of diagnosed problems (fever as a result of the flu) are not considered separate problems. Symptoms that are clustered around a known diagnosis are not counted separately.
Problem addressed: A problem is addressed or managed when it is evaluated or treated at the encounter by the physician or other qualified health care professional reporting the service. This includes consideration of further testing or treatment that may not be elected by virtue of risk/benefit analysis or patient/parent/guardian/surrogate choice.
Notation in the patient’s medical record that another professional is managing the problem without additional assessment or care coordination documented does not qualify as being ‘addressed’ or managed by the physician or other qualified health care professional reporting the service.
Referral without evaluation (by history, exam, or diagnostic study[ies]) or consideration of treatment does not qualify as being addressed or managed by the physician or other qualified health care professional reporting the service.
- This is an important clarification. How do we define “evaluated or treated?” When the condition is discussed in the history of the present illness and/or in the assessment and plan. Mentioning it “has a history of…” or the inclusion of it in the problem list does not meet the criteria of evaluated and treated.
- Example one: Internist sees a patient with CKD and notes, “managed by nephrologist.” This would not be counted as a problem on that date of service.
- Example two: Internist sees a patient with hypertension, and the need to change the hypertensive medication. The internists notes the creatinine level, and that she won’t prescribe a beta blocker because the patient has stage 3 CKD. This problem was evaluated and can be counted in the MDM calculation.
- If the clinician recommends a diagnostic test or treatment based on the risk/benefit analysis, but the patient declines the test or treatment, it is still counted.
- Referral without evaluation is not counted as a problem. “Patient wants a referral to the audiologist” isn’t sufficient. The HPI or exam or a discussion in the assessment would need to describe the patient’s hearing loss or tinnitus.
Minimal problem: A problem that may not require the presence of the physician or other qualified health care professional, but the service is provided under the physician’s or other qualified health care professional’s supervision (see 99211).
Self-limited or minor problem: A problem that runs a definite and prescribed course, is transient in nature, and is not likely to permanently alter health status.
- Unfortunately, CPT® does not provide any examples of this.
Stable, chronic illness: A problem with an expected duration of at least a year or until the death of the patient. For the purpose of defining chronicity, conditions are treated as chronic whether or not stage or severity changes (eg, uncontrolled diabetes and controlled diabetes are a single chronic condition). ‘Stable’ for the purposes of categorizing medical decision making is defined by the specific treatment goals for an individual patient. A patient that is not at their treatment goal is not stable, even if the condition has not changed and there is no short- term threat to life or function. For example, a patient with persistently poorly controlled blood pressure for whom better control is a goal is not stable, even if the pressures are not changing and the patient is asymptomatic. The risk of morbidity without treatment is significant. Examples may include well-controlled hypertension, non-insulin dependent diabetes, cataract, or benign prostatic hyperplasia.
- Stable is defined by the treatment goal. The meeting of the goal is not the “ideal” outcome, but meeting the goal for that patient.
- If the physician and patient have a treatment goal of an A1c level of 8, and the patient’s result is higher than that, the patient is not considered stable.
- A patient whose condition has not changed, and is not at their treatment goal, is not stable, even if the condition is the same as when last seen.
- CPT® emphasized the risk in the last sentence: the risk of morbidity without treatment is significant.
Acute, uncomplicated illness or injury: A recent or new short-term problem with low risk of morbidity for which treatment is considered. There is little to no risk of mortality with treatment, and full recovery without functional impairment is expected. A problem that is normally self-limited or minor, but is not resolving consistent with a definite and prescribed course is an acute uncomplicated illness. Examples may include cystitis, allergic rhinitis, or a simple sprain.
- These conditions have a low risk of morbidity and little or no risk of mortality without treatment
- This category includes self-limited or minor problems that are not resolving
Chronic illness with exacerbation, progression, or side effects of treatment: A chronic illness that is acutely worsening, poorly controlled or progressing with an intent to control progression and requiring additional supportive care or requiring attention to treatment for side effects, but that does not require consideration of hospital level of care.
Undiagnosed new problem with uncertain prognosis: A problem in the differential diagnosis that represents a condition likely to result in a high risk of morbidity without treatment. An example may be a lump in the breast.
- The key here is that the differential diagnosis includes a condition or illness with a high risk or morbidity without treatment.
- The example in guidelines is breast lump. The breast lump may turn out to be a benign condition, but breast cancer is in the differential diagnosis.
- Another example would be leg pain and redness after a procedure, with the patient scheduled for a doppler exam because DVT is in the differential diagnosis.
- The condition would likely lead to empiric treatment or diagnostic testing.
Acute illness with systemic symptoms: An illness that causes systemic symptoms and has a high risk of morbidity without treatment. For systemic general symptoms such as fever, body aches or fatigue in a minor illness that may be treated to alleviate symptoms, shorten the course of illness or to prevent complications, see the definitions for ‘self-limited or minor’ or ‘acute, uncomplicated.’ Systemic symptoms may not be general, but may be single system. Examples may include pyelonephritis, pneumonitis, or colitis.
- These are the same examples as in the original table of risk.
- Notice that general symptoms such as fever, body aches or fatigue in a minor illness are not considered here, as an acute illness with systemic symptoms.
Acute, complicated injury: An injury which requires treatment that includes evaluation of body systems that are not directly part of the injured organ, the injury is extensive, or the treatment options are multiple and/or associated with risk of morbidity. An example may be a head injury with brief loss of consciousness.
- Multiple injuries, not life-threatening.
- Fracture requiring evaluation of cardiovascular or neurovascular structures.
- Need to evaluate body systems not related to injury.
- Extensive injury.
- Multiple treatment options and/or treatment option associated with risk of morbidity.
Chronic illness with severe exacerbation, progression, or side effects of treatment: The severe exacerbation or progression of a chronic illness or severe side effects of treatment that have significant risk of morbidity and may require hospital level of care.
- CPT® has added the words “may require hospital level of care” to this definition.
- May require is not the same as will require and is admitted to the hospital.
Acute or chronic illness or injury that poses a threat to life or bodily function: An acute illness with systemic symptoms, or an acute complicated injury, or a chronic illness or injury with exacerbation and/or progression or side effects of treatment, that poses a threat to life or bodily function in the near term without treatment. Examples may include acute myocardial infarction, pulmonary embolus, severe respiratory distress, progressive severe rheumatoid arthritis, psychiatric illness with potential threat to self or others, peritonitis, acute renal failure, or an abrupt change in neurologic status.
- This is probably one of the most straightforward of the definitions, without significant disagreement about what it means.